Osteoarthritis
Osteoarthritis Basics
There are more than 100 types of arthritis and arthritis-related conditions. The term “arthritis” comes from the Greek words for joint and inflammation. More than 52 million adults and 300,000 children in the U.S. have some type of arthritis. The most common form of arthritis is the “wear and tear” type called osteoarthritis (OA), or Degenerative Joint Disease (DJD). Osteoarthritis most commonly affects the knees and hips.
About half of people over age 65 are diagnosed with OA, and the prevalence is dramatically increasing in middle aged people. About a third of those between age 50 and 65 have osteoarthritis, and this number is increasing.
Early Evaluation is Key!
Getting your bone and joint pain evaluated early is an opportunity to first determine the cause of your pain, and then develop a treatment plan to help you feel better and be more active. Early evaluation can potentially slow down the development of worsening arthritis. Even if you are seeing an orthopedic surgeon, there are many non-surgical and “in-between treatment steps to help. Many people are able to maintain an active lifestyle and reduce their pain with non-operative treatments.
Gender-Specific Differences in Osteoarthritis
There are important gender-based differences in OA that impact the development of the disease and success of treatments. Although 26% of women have arthritis (as opposed to 18% of men), women are three times less likely than men to have total joint replacement (TJR) surgery, despite having end stage degeneration. When women elect to have TJR, they are typically older and more frail, report worse arthritis pain, and have worse pre-op and post-op function scores.
Early evaluation of arthritis means that a gender-specific treatment plan can be developed. There are pain management options, specific exercises, and help with nutrition that are directly tailored for women experiencing painful arthritis. Many of these treatments can even help you safely and comfortably delay surgery.
What are the warning signs of arthritis?
There are several physical indicators that can let you know you might have arthritis:
Joint pain
Stiffness
Swelling and / or tenderness
Difficulty moving a joint
Crepitus or a “crunchy” sound with movement
Pain from Arthritis
For most people, coping with pain can be the hardest part of having arthritis. Pain can interfere with your ability to go about your daily tasks at home and work, and prevent you from resting and getting enough sleep. Although most people who have arthritis experience some degree of pain, pain is different for everyone and even differs between women and men. To understand arthritis pain, we should first look at its causes.
Pain can be caused by several things, including:
Inflammation/swelling from damage to the joint.
Stress on the joint due to muscle weakness, excess weight, or physical changes in the joint itself.
Emotional stress and fatigue can add to your pain.
Limited movement, stress, and depression can create a cycle of pain for arthritis sufferers, making it all the more difficult to deal with.
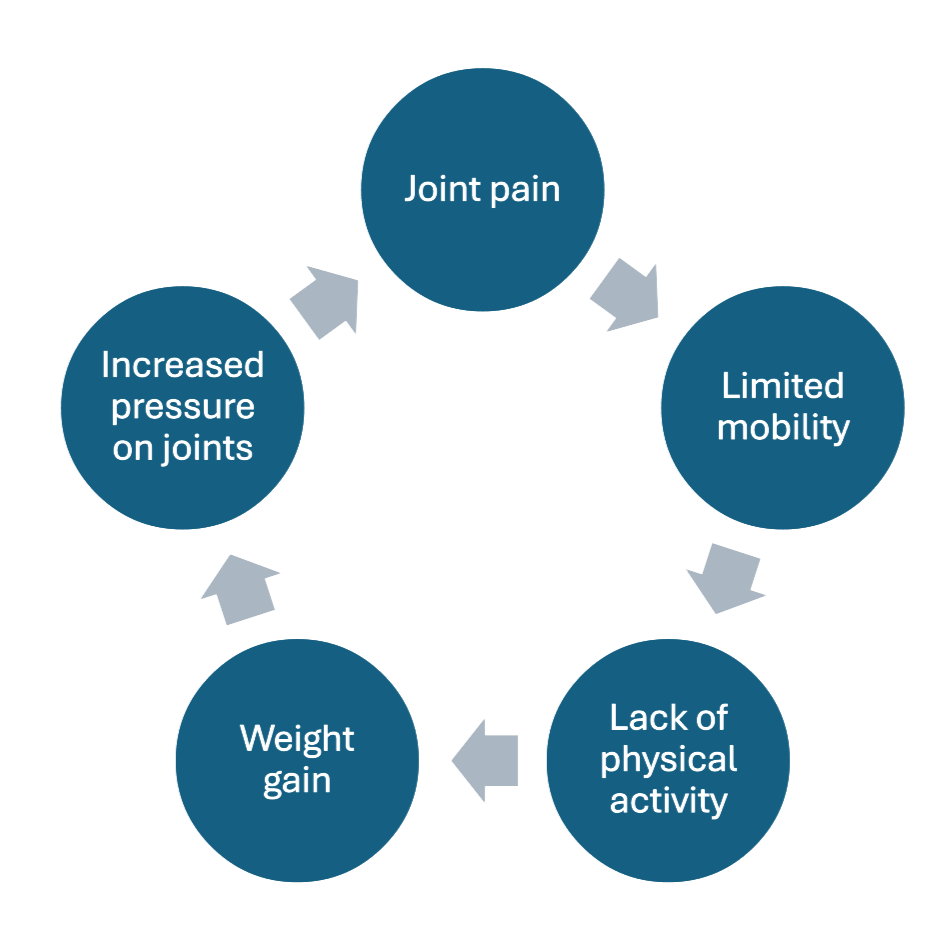
Arthritis Pain and the Vicious Cycle
Osteoarthritis causes joint pain that makes it harder to move. When you move less due to joint pain, you are likely to gain weight (adding more stress to the joints and increasing pain even more). When you gain weight, co-morbid conditions like heart disease, diabetes, and depression often worsen. Worsening health makes it even more difficult to move and the cycle continues. Women – especially African American and Latina women – are the most likely to suffer from these effects.
Types of Pain
There is more than one type of pain. Pain can be “acute" or “chronic.” Acute pain is pain that has been present for less than 3 months and tells you that you need to act. It is severe and usually lasts a shorter time. Chronic pain is pain that lasts longer than 3 months, like the kind that accompanies arthritis. Chronic pain isn’t as easy to relieve as acute pain, and over time it can become difficult to treat. The result is what we call “chronic pain syndrome” where it seems impossible to escape the pain. Managing this type of pain is critical to improving your quality of life.
Arthritis pain is not the same for everyone. In addition to the different types of pain, there are different interpretations of pain. Your pain may vary from day to day and affect different joints or body parts on any given day. Women, men, and people of different races are all impacted by pain in different ways, and require personalized approaches to managing their pain. What works for one person might not work for someone else, so creating a personal pain management plan is critical.
Treatment Options for Osteoarthritis
The Best Treatment Starts with Early Evaluation
In addition to joint replacement surgery, there are many effective non-operative treatments. Not all patients need to start with surgery because arthritis is not “all or nothing.” It progresses over time. Developing a treatment plan that works for you is critical.
Arthritis treatment is aimed at reducing pain and restoring function and mobility. Early evaluation is key to successful outcomes whether you are choosing operative or non-operative treatments. Your first arthritis evaluation will include medical and medication histories, X-rays, a physical exam of the joint(s) bothering you, and questions about your pain including its location and to what degree it affects your mobility and functioning.
Operative Treatment (Surgery)
The decision to have surgery is based upon the severity of arthritis and how badly it is affecting your quality of life and function. It is always best to start with nonoperative treatments, even if you’re planning to have surgery. For more information that will help you decide if surgery is right for you, visit pittsburghboneandjoint.com.
Non-Operative Treatments
Non-operative treatments can be very effective in reducing pain, increasing mobility, losing weight, and breaking out of the vicious cycle. Movement, nutritional support, joint injections, and more can help you manage the pain you’re having and slow the progression of OA.
Non-Operative Treatments for OA
Movement is medicine for joint pain. Exercise plans should include cardiovascular, strengthening, and stretching for weight management and stability.
Start your exercise plan with safe and accessible physical activities like the Move to Mobility program. Consult an expert if needed.
Include strength-training, stretching, balance, and cardiovascular activities. Walking and tai chi are good options that cover multiple types of exercises and provide both pain reduction and bone building benefits.
Aim for 30 minutes a day of moderate intensity movement. If 30 minutes is difficult for you, try to doing 10 minutes of movement three times a day.
All movement counts and will provide health benefits. Remember things like taking the stairs, walking to the mailbox, house/yard work, and dancing when creating your movement goals.
Use heat and ice (heat before movement, ice after movement) to manage pain.
Exercises may be different for women and men. The Wellness Center can help you find activities that are safe and effective for you.
Joint Injections
Joint injections are potent anti-inflammatories that are meant to reduce pain and restore function and mobility to the joint so that you can move more. The injections stay inside your knee or hip joints which can be very effective in relieving pain, often times for several weeks or months. There are several types of joint injections that can help manage pain caused by arthritis. Work with the Wellness Center and your orthopaedic care team to determine if you are a candidate for injections.
Cortisone/Corticosteroid injections work by treating the inflammation that causes pain and swelling.
Effects can last from 3 to 12 months and sometimes longer.
All insurances cover this injection.
Since this injection is a steroid medicine, it has a higher efficacy for bone on bone (end stage) joints.
Hyaluronic acid injections deliver lubricating fluid into the joint. The goal is to temporarily lubricate the joint, thereby decreasing painful inflammation and improving function.
For this injection to have any anti-inflammatory effect, at least some cartilage must still be present in the joint.
When the joint is bone on bone, there is little to no pain-relieving effect from these lubricating injections.
Platelet-rich plasma (PRP) injections are an additional non-operative treatment for pain caused by knee and hip arthritis and hip bursitis.
PRP is a “biologic” and potent anti-inflammatory treatment.
PRP is the separation of platelets (part of blood responsible for clotting) and plasma from the rest of the blood, resulting in a high concentration of platelets within the plasma.
PRP is considered a “natural” treatment since it is derived from your own blood. You can get PRP injections frequently. There is no limit of PRP that you can receive.
PRP injections can be used in concert with other injections like the steroid and lubrication injections, and may reduce the need for oral anti-inflammatory drugs.
Cryoanalgesia uses cold to disrupt the pain transmitting portion of nerves and produces an immediate, long-lasting “block” of the pain sensors, leaving muscle function intact.
The treatment (Iovera System) uses a series of superficial treatments with small needles that apply cold to a specific nerve, creating a small ice ball just underneath the skin. This immediately stops the nerve from sending pain signals.
The effect on the nerve is temporary and does not cause permanent damage.
The pain relief can last as long as 6 to 9 months and can be repeated at 3 month intervals if needed.
Nutritional Support
Nutrition should focus on foods that reduce inflammation, support muscle growth, and protect bone density. Keeping a balanced diet will also help you reach and maintain a healthy weight and reduce stress (and pain) on your joints. Excess body fat leads to painful inflammation and adds pressure to joints, so every pound of body weight feels like 4 pounds of weight on the knees. Follow these nutrition tips for bone and joint health:
A diet rich in anti-inflammatory ingredients and tissue-building protein will fuel your body for movement and reduce pain-causing inflammation. Think of the “Mediterranean diet.” The Wellness Center can give you our “Nutritional Support” materials for more help with an anti-inflammatory style of eating.
Avoid highly-processed meats, refined grains, and food that contain them like many snack foods and white bread. Instead, choose whole fruits and vegetables and lean meats.
Eliminate or reduce trans fats, and limit saturated fats. Look instead for mono- and poly-unsaturated fats.
Sugar causes inflammation, so reduce added sugars and limit sweets.
Increase omega-3s like olive oil, walnut oil, salmon, and sardines.
Non-Narcotic Medications
Non-narcotic medications can include oral medications like acetaminophen and NSAIDS, and topical medications. These medications can be helpful in reducing pain and inflammation. Work the your Wellness Center to determine which medications are safe for you.
Sleep
Pain from arthritis can interrupt your sleep, and poor sleep can make pain worse (known as “painsomnia”). There are things you can do to improve your sleep:
Move every day. Physical activity contributes to more restful sleep.
Establish a healthy sleep routine. Go to bed and get up at the same time every day, even on weekends.
Take a warm bath or shower before bed to soothe and relax your system.
Keep your bedroom dark and cool.
Avoid alcohol. It may help you fall asleep, but it disrupts the sleep cycle.
Use pillows to support painful joints and keep your body in alignment. An occupational therapist can suggest sleep positions that are effective.
Stress and Anxiety Reduction
Mindfulness and other stress reduction techniques have been shown to reduce how people experience pain.
Movement is medicine! Exercise has been shown to increase your body’s “feel good” hormones.
Deep breathing - a quick, simple technique - reduces stress, inflammation, and pain.
Use a journal or diary before bed to write about something good from your day. When you need a pick-me-up, reread your notes.
Meditate by focusing on the present moment and letting go of distractions and negative thoughts. Try using an app like Headspace or Calm.
Get outside for movement, quiet, and vitamin D.
Socialize with people you enjoy being around.
Consider speaking with a therapist or trained professional if you need additional help managing stress.
Other Ways to Soothe and Protect Painful Joints
Simple and natural ways to reduce pain and stiffness and improve function include:
Movement: Joints want to move! Inactivity will make joint pain worse!
Heat: Use a heating pad or warm bath or shower to increase blood flow to painful joints and relax the surrounding muscles. Apply heat for no more than 15 - 20 minutes at a time.
Cold: Use cold packs or ice packs to numb the area and reduce swelling. Place a towel or other barrier between the cold and your skin. Apply for 15 - 20 minutes at a time.
Adaptive devices: Canes, walkers, splints, and braces can help you move safely and maintain mobility.
Stretching: Gentle stretching will soothe aching joints, even on painful days.
Physical or Occupational Therapy: Work with a physical or occupational therapist to modify daily tasks such as unloading the dishwasher or dryer or even turning a doorknob. Physical and occupational therapists can help you determine the safest ways to maintain your independence at home. The Wellness Center can help you find a PT/OT that is right for your needs.
Additional Resources
OA affects many areas of your life and health, and it can be hard to know where to start. The Wellness Center for Bone and Joint Health understands the complexities of OA and knows that your wellness is more than just pain management. We can help you with:
Gender-specific issues and treatments
Osteoporosis screenings and prevention
Reducing the risk of falling
Important medication reviews
Pain management through non-medication based therapies